While Avascular Necrosis (AVN) might not be a household term, it’s a condition that can significantly impact your health, particularly in your bones and joints. Just like with many health issues, catching AVN early is key.
If we detect it early, we have a better chance of stopping it from causing severe damage to our bones and joints. You must know what it is, what causes it, and what you can do to stay as healthy as possible. Education is the first step in taking control of your health, and that’s what we’re here to do!
What is Avascular Necrosis?
Avascular Necrosis, often abbreviated as AVN, is a medical condition you might also hear referred to as Osteonecrosis. But what does this mouthful of a term mean?
At its core, AVN/Osteonecrosis is all about the health of your bones and, more specifically, what happens when that health gets compromised. You see, bones are living tissues, and just like any other part of our body, they need a good supply of blood to stay alive and function correctly.
AVN is a condition where the blood supply to a particular bone is disrupted, leading to a cascade of problems we’ll get into shortly.
Causes of Avascular Necrosis
Common Risk Factors
1. Trauma and Injury
One of the more common culprits behind Avascular Necrosis is trauma or injury to a bone. When a bone is fractured or dislocated, it can disrupt the blood supply to that area. This interruption in blood flow can set the stage for AVN to develop.
2. Chronic Steroid Use
While valuable for various medical conditions, steroids can have side effects when used for prolonged periods. One of these side effects is the potential to affect the blood supply to the bones. Chronic steroid use, whether for autoimmune diseases or other conditions, can increase the risk of AVN.
3. Alcohol Abuse
Excessive alcohol consumption can harm not only your liver but also your bones. It can directly impact blood vessels, decreasing blood flow to the bones. Over time, this can contribute to AVN, especially in the hip.
4. Certain medical conditions (e.g., sickle cell disease)
Some medical conditions, like sickle cell disease, can lead to abnormal red blood cells that struggle to flow through blood vessels. This can result in blockages in the small blood vessels supplying bones, making individuals with such conditions more susceptible to AVN.
Less Common Risk Factors
1. Radiation Therapy
Radiation therapy is a vital cancer treatment, but it can have unintended consequences. In some cases, radiation therapy near a bone can damage blood vessels, impairing blood supply and potentially triggering AVN.
2. Blood clotting disorders
Disorders that affect blood clotting can increase the risk of clot formation within blood vessels. If a clot obstructs blood flow to a bone, it can initiate the development of AVN.
Symptoms and Diagnosis of Avascular Necrosis
Early Signs and Symptoms of AVN
1. Joint Pain
The early stages of Avascular Necrosis often go unnoticed, but one of the telltale signs is joint pain. This pain can be persistent, deep, and may start gradually. Initially, it might be mild and intermittent, often mistaken for common aches. However, the pain can become more intense and persistent as AVN progresses.
2. Limited Range of Motion
AVN affects the bone’s structural integrity and can limit your joint’s range of motion. Moving your affected joint as freely as before may be difficult. Simple actions like bending a knee or raising an arm can become challenging and uncomfortable.
How AVN Progresses
Understanding how AVN progresses is crucial because it can help you gauge the severity of the condition and the urgency of seeking treatment. As the blood supply continues to be compromised, the bone tissue begins to break down.
This process can lead to small fractures and the eventual collapse of the bone. In essence, untreated AVN can escalate from minor discomfort to debilitating joint damage, significantly impacting your quality of life.
Diagnostic Methods
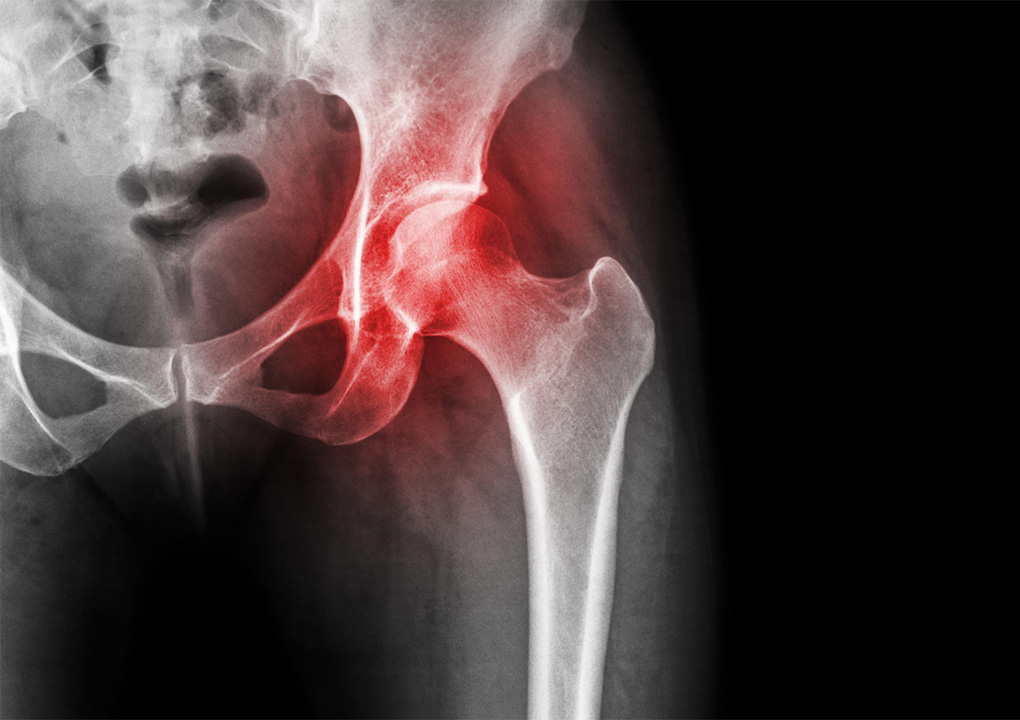
1. X-Rays
X-rays are often the first line of diagnostic imaging for AVN. They can reveal changes in bone structure, including areas of bone damage and collapse. However, X-rays may only sometimes detect AVN in its very early stages.
2. MRI Scans
Magnetic Resonance Imaging (MRI) scans are highly effective in detecting AVN, even in its early stages. MRI provides detailed images of bone and soft tissue, allowing healthcare professionals to assess the extent of bone damage and plan appropriate treatment.
3. Bone Scans
Bone scans involve injecting a small amount of radioactive material into your bloodstream. This material accumulates in areas of increased bone activity, which can help identify regions affected by AVN. Bone scans are especially useful for detecting AVN in its early stages.
Common Sites of Avascular Necrosis
Hip Joint AVN
Knee Joint AVN
Shoulder Joint AVN
Other Affected Areas
It’s important to note that AVN can affect any bone in the body, though it’s less common in certain areas. Some other bones and joints that AVN can impact include:
- Ankle joint: AVN in the ankle can lead to pain and difficulty walking.
- Wrist joint: AVN in the wrist can cause discomfort and reduced hand function.
- Elbow joint: AVN in the elbow can result in pain and limited arm movement.
- Jawbone: AVN in the jawbone can lead to jaw pain and difficulties with chewing.
Treatment Options for Avascular Necrosis
Non-surgical Approaches
1. Medications For Pain Management
Pain relief is a crucial aspect of AVN treatment. Over-the-counter pain relievers or prescription medications can help manage the discomfort associated with AVN. In some cases, medications may also include drugs to slow the progression of AVN by improving blood flow to the affected bone.
2. Physical Therapy
Physical therapy plays a pivotal role in AVN management. A physical therapist can design a customised exercise program to improve joint function, strengthen muscles, and reduce pain. These exercises help maintain joint mobility and reduce the risk of complications.
Surgical Interventions
1. Core Decompression
Core decompression is a surgical procedure primarily used in the early stages of AVN, especially for hip joint AVN. It involves drilling a hole into the affected bone to relieve pressure and stimulate the formation of new blood vessels. This could slow down or stop the progression of AVN.
2. Bone Grafting
In cases where AVN has already caused significant bone damage, bone grafting may be necessary. During this procedure, healthy bone tissue is transplanted from one part of the body (or a donor) to the affected area. This helps to strengthen the bone and promote healing.
3. Total Joint Replacement
Total joint replacement is considered when AVN has led to severe joint damage and pain that can’t be managed through other methods. In this procedure, the damaged joint is removed and replaced with an artificial joint (prosthesis). Total joint replacement can significantly improve joint function and reduce pain.
Choosing the Right Treatment Plan
Rehabilitation and Recovery
Lifestyle Changes and Prevention of Avascular Necrosis (AVN)
Lifestyle Modifications for AVN Patients
1. Weight Management
Maintaining a healthy weight is crucial for AVN patients, especially for those with weight-bearing joint involvement like the hips and knees. Excess body weight can place added stress on already compromised joints, exacerbating pain and further damaging the affected area. Consult with your healthcare provider to establish a weight management plan tailored to your needs.
1. Weight Management
Maintaining a healthy weight is crucial for AVN patients, especially for those with weight-bearing joint involvement like the hips and knees. Excess body weight can place added stress on already compromised joints, exacerbating pain and further damaging the affected area. Consult with your healthcare provider to establish a weight management plan tailored to your needs.
2. Limiting Alcohol and Tobacco Use
If you’re dealing with AVN, it’s essential to limit or, ideally, abstain from alcohol and tobacco. Both alcohol and smoking can adversely affect blood circulation, which is already compromised in AVN. These substances can exacerbate the condition and hinder your body’s natural healing processes.
3. Exercise and Joint-Friendly Activities
While rest is essential during AVN treatment and recovery, physical activity remains crucial. Consult with a physical therapist to develop an exercise program tailored to your condition. These exercises can help maintain joint mobility, strengthen supporting muscles, and improve overall joint health. Opt for low-impact activities like swimming or cycling, which put less stress on your affected joints.
Prevention Strategies for Those at Risk
1. Early Treatment of Underlying Conditions
If you have medical conditions known to increase the risk of AVN, such as sickle cell disease or certain clotting disorders, it’s crucial to manage these conditions effectively. Follow your healthcare provider’s recommendations, adhere to prescribed treatments, and attend regular check-ups to catch any potential complications early.
2. Avoiding Excessive Steroid Use
If you’re prescribed steroids for any medical condition, use them only as directed by your healthcare provider. Avoid prolonged or excessive steroid use, as this can increase the risk of AVN. If you have concerns about your medication regimen, discuss them with your healthcare provider to explore alternative treatments or strategies.
3. Injury Prevention
Trauma and injuries can trigger AVN, so preventing accidents is essential. Wear appropriate safety gear during sports and physical activities, and be cautious in environments where falls or accidents are more likely. Falls can cause fractures and damage blood vessels, potentially leading to AVN in the affected area.